Acid-Base Disturbance
Instructions:
Solution.
How would you classify the patient’s acid-base disturbance and explain why?
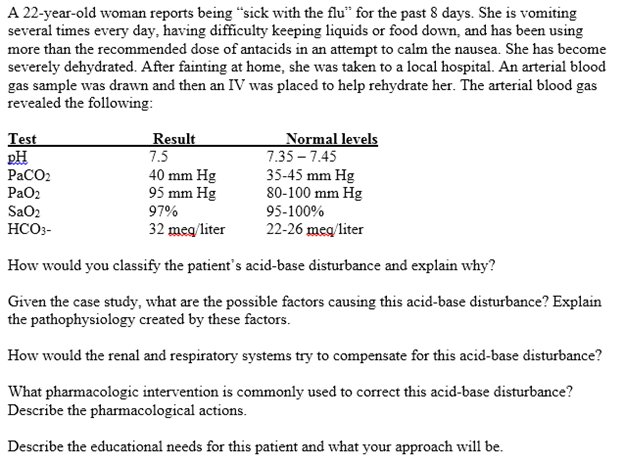
As compared to the normal values of arterial substance, the patient has a high pH of 7.5, a high arterial HCO3– concentration of 32 meq/liter, and a normal arterial partial pressure of carbon dioxide. This combination suggests that the patient is experiencing metabolic alkalosis. the high pH and the high bicarbonate concentration in the blood is a clear indication that the blood is alkaline. As opposed to respiratory alkalosis, which results from an increase of blood levels of carbon dioxide, metabolic alkalosis results from a high blood concentration of bicarbonate, which is evident in the patient’s results (Gennari, 2011).
Given the case study, what are the possible factors causing this acid-base disturbance? Explain the pathophysiology created by these factors.
The patient’s metabolic alkalosis has been contributed towards by two major factors, the loss of hydrogen ions through vomiting and the excessive intake of non-absorbable antacids. To start with, vomiting leads to the elimination of gastric juices from the body, which have high amounts of hydrochloric acid (Gennari, 2011). The loss of each hydrogen ion from the extracellular space leads to the gain of a bicarbonate ion. An increase in the bicarbonate ions in the patient’s extracellular blood as a result of the patients persistent vomiting led to the loss of acidity within the blood and hence the development of metabolic alkalosis.
On the other hand, antacids are alkaline in nature as they are consumed as acid neutralizers. Hence, by consuming high amounts of antacids above the recommended dosage, the patient increased the concentration of bicarbonate in the blood upon absorption. In this case, the non-absorbable antacids, such as magnesium hydroxide, aluminum, or calcium with base carbonate or hydroxide, contains anions that buffer hydrogen ions found in the gastric juices (Łoniewski & Wesson, 2014). On the other hand, the bicarbonate produced in the pancreas is bound by the cation, an aspect that results in bicarbonate loss via stools. In most cases, such a process leads to the loss of both bicarbonate and hydrogen ions, hence no disturbance of the acid-base balance is observed. Nevertheless, in some cases, some of the bicarbonate is not bound by the consumed cation, which results in the absorption of such bicarbonate amidst the loss of hydrogen ions (Łoniewski & Wesson, 2014). This leads in an increase in the level of bicarbonate in the arterial blood as compared to a low level of hydrogen ions. This interference with the balance established by the body between the acid level and the basic level of the blood, led to the development of alkalosis.
How would the renal and respiratory systems try to compensate for this acid-base disturbance?
To compensate the metabolic alkalosis observed in the patient, the respiratory system would attempt to retain more carbon dioxide in the body. Lungs control the amount of carbon dioxide found in the blood. This carbon dioxide combines with water forming carboxylic acid (H2CO3). With the increase in the levels of bicarbonate in the body, chemoreceptors found in the brain would respond to the resultant pH change, thus alter the depth and rate of respiration to control the levels of CO2 (Feldman, Alvarez, Trevino, & Weinstein, 2012). In this case, the chemoreceptors would slow down the rate of breathing and make breaths shallow, an aspect that would lead to high retention of CO2 in the blood, hence cause and increase in hydrogen ions, which would displace bicarbonate ions and establish an acid-base equilibrium. On the other hand, the renal system promotes a balance in the body’s acid-base status by excreting or absorbing bases and acids. In the case of metabolic alkalosis, the patient’s kidneys would restore balance by retaining H+ ions through reabsorption and excreting HCO3– (Seifter, 2014). The bicarbonate reabsorption mechanism is reversed in this case, allowing more bicarbonate to be eliminated from the body in order to reduce the alkalinity of the blood.
What pharmacologic intervention is commonly used to correct this acid-base disturbance? Describe the pharmacological actions.
Treatment of metabolic alkalosis highly relies on the etiology of the conditions. In this case, the patient’s condition was as a result of vomiting and excessive intake of non-absorbable antacids. As such, the most common treatment in this case is to administer antiemetics, which reduce vomiting and hence the loss of hydrogen ions present in the gastric juices (Seifter, 2014). Dilute hydrochloric acid may also be administered intravenously in case of an emergency to increase the level of hydrogen ions in blood. Nevertheless, it is important to watch out for hemolysis, which is a major risk of intravenous HCL.
Describe the educational needs for this patient and what your approach will be.
The patient needs to be educated on the proper use
of antacids and the various problems that may be encountered if consumed in
excess or alongside other alkaline substances. It is also important for the
patient to be educated on proper dietary behavior in order to ensure a
reduction in the consumption of foods that are high in sodium carbonate. To
effectively educate the patient, it is important to initiate patient-centered-care
as this would provide an avenue for understanding any other factors that
contribute to the patient’s problems such as vomiting. Creating a rapport with
the patient would allow for a proper interpersonal relationship and encourage
the patent not only to open up, but to trust the nurse. This would lead to proper
understanding of the provided information and increase chances of compliance.
References
Feldman, M., Alvarez, N. M., Trevino, M., & Weinstein, G. L. (2012). Respiratory compensation to a primary metabolic alkalosis in humans. Clinical nephrology, 78(5), 365-369.
Gennari, F. J. (2011). Pathophysiology of metabolic alkalosis: a new classification based on the centrality of stimulated collecting duct ion transport. American Journal of Kidney Diseases, 58(4), 626-636.
Łoniewski, I., & Wesson, D. E. (2014). Bicarbonate therapy for prevention of chronic kidney disease progression. Kidney international, 85(3), 529-535.
Seifter, J. L. (2014). Integration of acid–base and electrolyte disorders. New England Journal of Medicine, 371(19), 1821-1831.

