Depression in the Adolescent
Instructions:
To prepare:
• Reflect on depression in the adolescent.
• Think about the epidemiology of the issue.
• Consider an age-appropriate protocol for the diagnosis, management, and follow-up care of the issue you selected.
• Think about how culture might impact the care of patients that present with this issue.
To complete:
Write a 2- to 3-page paper that addresses the following:
• Explain a growth and development or psychosocial issue that might present in adolescents. Include the epidemiology of depression in adolescents in your explanation.
• Explain an age-appropriate protocol for the diagnosis, management, and follow-up care of this issue.
• Explain how culture might impact the care of patients who present with the growth and development or psychosocial issue you selected.Week 4 Paper Instructions
1. Explain the selected disorder in the selected age-group including:
A. An explanation of what depression is and how it affects the adolescent.
B. A discussion on the epidemiology, specifically as it relates to adolescents. Epidemiology includes: 1) The incidence, distribution, and control of disease in a population. AND 2) The sum of the factors controlling the presence or absence of a disease or disorder.
2. Explain a protocol for the diagnosis, management, and follow-up care for depression.
A. Protocol is defined as a detailed plan. In this paper, just as in the last, you are expected to develop an evidence-based protocol that can be used to inform the diagnosis, management, and follow-up related to your selected topic.
B. You must include, SPECIFICS, directing and informing the clinician on how depression should, in the primary care setting, be: 1) Diagnosed (this includes what to look for, symptoms, diagnostic testing, etc.); 2) Managed, which includes SPECIFIC treatment options to include medication therapy, other therapies, referrals, etc; 3) Followed, including the frequency, purpose, and plan for follow-up visits.
3. Explain how culture might impact the care of patients who present with depression. This means you will discuss:
A. How CULTURE and cultural barriers may impact depression specifically (not random groups of people, certain minority groups, or families in general, but CULTURE). Please remember, America is a cultural melting pot! AND
B. Specific strategies the clinician should utilize to overcome these barriers to ensure the patient is properly cared for. Remember, we are focused on PROPER CARE of the patient. For example, if you tell me that certain cultural practices are considered child abuse in this country, it is not appropriate for you to tell me in your protocol that you should over look this because it is a cultural thing. That would be the incorrect response
Solution
Depression in the Adolescent
Introduction
The DSM-V suggests that a depressive disorder as a condition that an individual experiences either loss of interest or pleasure in doing something or a ‘depressive mood’ within the two weeks of observance coupled with a change in the standard functionality of an individual such as self-image, eating habits, sleep patterns and concentration levels (American Psychiatric Association, 2013). As such statistics suggest that most of the American teens experience periods of major depression. Major depression is a common disorder in adolescents, and it is advised that they should seek medical attention to avoid the severity brought about with it. As such, this essay transcends a discussion of depression in adolescents, its prevalence, diagnosis and treatment plan as well as the impact of culture on the treatment of depression.
Epidemiology
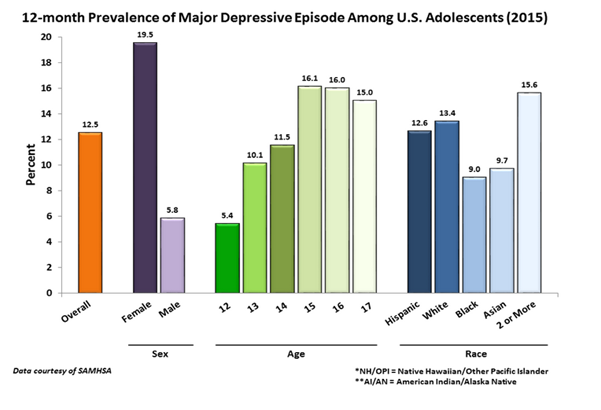
Statistics suggest that 19. 5 percent of female adolescents, aged 12-17, in America experience major depressive episodes during their adolescent age. Overall, statistical data in the year 2015 dictates that 3,000,000 adolescents of age 12-17 years in the US experience at least a single depressive episode (NIMH, 2015).
The figure below shows the epidemiological studies, in 2015, on major depression among US adolescents. The data is adapted from the National Mental Health Institute, courtesy of the Substance Abuse and Mental Services Administration (SAMHSA).
Causative factors of Depression in Adolescents
Scholars suggest that there is no confirmed cause of depression in adolescents (Goldstein & Rosselli, 2003). As such they suggest that depression if triggered by a number of factors. First, traumatic life events such as loss of a beloved one, physical/emotional abuse or sexual assault can trigger depression. Second, it suggested that depression has a biological constituent, per se; children who have relatives (parents) that have experienced depression are more prone to developing a depressive disorder. Finally, it is imperative to note that the differences in the brain structures of adolescents which are characterized by fluctuating levels of neurotransmitters can trigger stress more easily in teenagers than in adults (Bress, Meyer, & Hajcak, 2015).
Diagnosis and Symptoms
As mentioned earlier, the DSM-V suggests that a teenager must meet the DSM criteria to be diagnosed with major depression. As such it stipulates that an individual must satisfy at least two major episodes of depression for a period of two weeks. These episodes must encompass the following symptoms;
- Signs of agitation or retardation that is noticeable by peers.
- Daily depressive moods.
- Diminished interest in daily activities as well as ability to concentrate.
- Fatigue
- Feelings of unwarranted guilt and ineptitude.
- Insomnia and irregular sleeping patterns.
- Frequent suicidal thoughts.
- Rapid weight loss.
Treatment and Prognosis
Depression is treated with both drug therapy and psychotherapy. Drug therapy involves medication by a physician, which directs the patient to take manufactured drugs to reduce the levels of depression. First, the use of selective serotonin reuptake inhibitors is one of the effective antidepressant medicines. SSRIs tend to have fewer side effects, and they work on the regulation of the serotonin levels in the brain. Such drugs include; Paxil, Pexeva, Prozac, Lexapro, among others. Second, selective serotonin and norepinephrine reuptake inhibitors can be used to alter the re-absorption of serotonin and norepinephrine which aid in the regulation of mood. Its side effects include headaches, vomiting, insomnia, and constipation (Thase & Schwartz, 2015). The most common SNRIs are duloxetine and venlafaxine. The other drug therapies include the use of the tricyclic antidepressants and use of monoamine inhibitors. All the drugs within depression treatment must be approved by the Food and Drug Administration (FDA)
Alternatively, psychotherapy entails a visit to a qualified mental health practitioner before or during drug therapy. Psychotherapy methods include the use of cognitive-behavioural therapy, talk therapy, psychodynamic therapy and problem-solving therapy. These treatments help in restructuring the cognitions in an individual and assist in alleviating internal conflicts as well as reducing stress levels (Busch, Rudden, & Shapiro, 2016).
Culture and Treatment of Depression
America
has a diverse culture, as such, practitioners are
faced with difficulties in the treatment and diagnosis of depression due
to lack of cultural competence. The possible cause of cultural impacts results
from collectivism, acculturation, and
gender (Alegría, et al., 2015). Notably, stigmatization
is one of the effects of cultural
perceptions of the disorder. Despite the
fact that depression is classified as a
mental disorder, most cultures in the US believe that depression should not
require any form of medication. For example, cultures that originate from Asia
describe symptoms of depression as a physical complaint. Therefore it would be
difficult for healthcare professional to administer treatment. It is suggested that the use of the
biopsychosocial model as an appropriate method to eliminate stigmatization and
make the populace to be aware of the mental illness (Khan, Asghar, Mukhtar, & Niaz, 2016).
References
Alegría, M., Chatterji, P., Wells, K., Cao, Z., Chen, C. N., Takeuchi, D., & Meng, X. L. (2015). Disparity in depression treatment among racial and ethnic minority populations in the United States. New York: Psychiatric services.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publications.
Bress, J. N., Meyer, A., & Hajcak, G. (2015). Differentiating anxiety and depression in children and adolescents: Evidence from event-related brain potentials. Journal of Clinical Child & Adolescent Psychology, 44(2), 238-249.
Busch, F. N., Rudden, M., & Shapiro, T. (2016). Psychodynamic treatment of depression. American Psychiatric Publications.
Goldstein, B., & Rosselli, F. (2003). Etiological paradigms of depression: The relationship between perceived causes, empowerment, treatment preferences, and stigma. Journal of Mental Health, 12(6), 551-563.
Khan, M., Asghar, S., Mukhtar, Z., & Niaz, S. (2016). Biopsychosocial model of prevention of depression. European Psychiatry, 33, S177.
NIMH. (2015). Major Depression Among Adolescents. Retrieved December 24, 2016, from National Institute of Mental Health: https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adolescents.shtml
Thase, M. E., & Schwartz, T. L. (2015). Choosing medications for treatment-resistant depression based on mechanism of action. The Journal of clinical psychiatry, 76(6), 720-727.

