Minimizing Readmissions through Workflow Analysis
Instructions:
Write a workflow analysis summary. This summary should detail your proposed new healthcare technology system. Determine how new information systems will be developed, integrated, and interoperable in healthcare.The summary should describe how your new information technology could address one or more of the workflow problems identified in your organization/department among healthcare professionals -nurse- provider-patient. PROBLEM: Readmission rates in U.S. hospitals are a continued focus. Patients are sent home without a complete understanding of their medications, treatment plans, or other discharge instructions, including provider follow-ups. Any technology solutions to keep patients engaged in their care post discharge? Could such a system exist in the inpatient environment as well as in the home? What does the current state look like and what would the future state look like post implementation of a new system? Make sure to not only identify what the information technology is, but also how it will improve nurses workflow and clinical or administrative outcomes. In addition, this assignment requires you to include workflow diagrams. Using the flowchart symbols within Microsoft PowerPoint (or other process mapping software), develop 2 flowcharts: one of the current state workflow prior to your new solution and another representing the future state, post implementation. These charts should be embedded into your workflow analysis summary in the appropriate logical position.
Your work analysis includes: 1) The impact of information technology 2)Workflow diagrams 3)Issues and problems 4) Solutions (You present a brilliant potential technology solution to correct the issue from nurses view). 5) Evidence
Your workflow analysis summary should include a minimum of 2 scholarly references that support your technology solution and/or the workflow methodology
Solution.
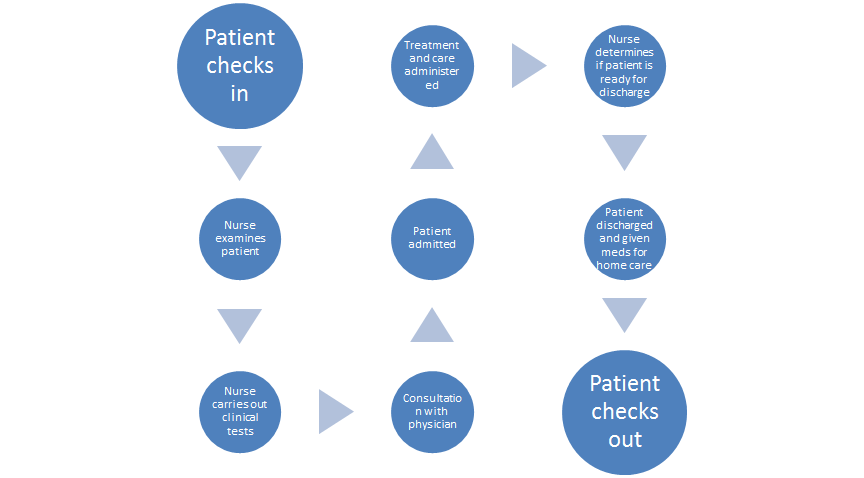
Current workflow
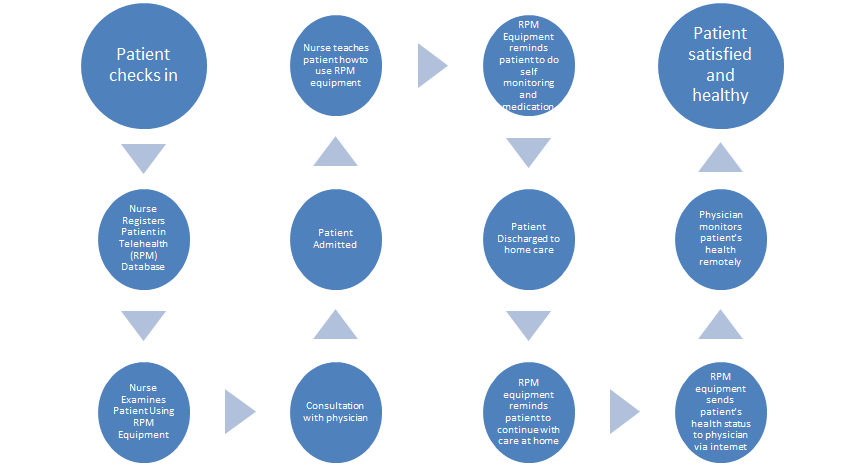
Workflow after implementation of Telehealth
Minimizing Readmissions through Workflow Analysis
In the US, there is currently a high rate of readmission in hospitals. Regulations have been put in place that attempt to minimize the rates, including the Affordable Care Act (ACA), which came into force in 2004. However, to date, the rates have not had significant reductions. The Act was made to enforce penalties on hospitals that have excess rates of readmissions. Research has shown that majority of the readmissions are preventable. The rates declined, but only slightly. One of the reasons for the increase in the readmission rates is the lack of proper health technology to help maintain coordination between health professionals, nurses, health providers and the patient. Patients are discharged before they clearly understand the details of home based care and the post discharge instructions. Some patients therefore end up neglecting the instructions thereby worsening their conditions, leading to repeated admissions before 30 days are over (McGonigle, & Mastrian, 2015).
At Grace Ministries Hospital, where I work, patients arrive and check in at the reception desk, they are referred to the examination and consultation points. The patient gives vital information about him/herself, which is recorded by the provider and the patient is entered into the computer system. The patient is then referred to the physician’s office where the physician views the patient’s information and determines whether the patient needs to be admitted or not. The doctor then sends the patient off with a prescription list, which is used by the provider to admit the patient and the nurse commences treatment. The patient is later discharged upon the judgment of the nurse.
This type of workflow has many loop holes that can lead to preventable readmissions. The fact that the patient moves throughout the system unaided leads to patient dissatisfaction with the treatment process. Dissatisfied patients don’t heal quickly in many cases. They are more likely to have readmissions than satisfied ones. The fact that patients are discharged at the judgment of the nurse poses the risk of discharging a patient who is not yet ready for home-based care. The patient may not understand the rules of home-based care and therefore leading to a readmission (McGonigle, & Mastrian, 2015).
A proper solution to these problems is the implementation of Telehealth, Remote Patient Monitoring (RPM) program. The system involves the use of technology equipment that can help the patient take medication and monitor his or her health. The devices are given to the patient while still admitted and the patient is taught by the nurse on how to use them. Among the health monitoring activities are: body weight measuring each day, body temperature, measurements of blood pressure and other health conditions relevant to the patient’s disease. The RPM device is programmed to send the information about the measurements to the physician via internet. The physician uses the information to monitor the patient and address any new health complications that may arise (Center for Connected Health Policy (CCHP), 2016).
If Telehealth is implemented by the hospital, there are many benefits the health professionals, nurses, provider and patient will get. The health providers will be able to admit more patients and therefore help cure more diseases. They health centre will also be able to free more bed space by sending off patients who quickly master how to use the RPM device. Since patients who are still admitted can also use the device to take care of themselves, the nurses will have time to help other patients who need their help. The physicians are able to take care of their patients and remedy any new conditions even after they are discharged thereby minimizing readmissions and maximizing patient recovery and satisfaction. The patients also get the benefit of receiving maximum care within the setting of their homes. They also do not have to travel to the hospital every time they feel unwell or notice any condition that requires the physician’s attention (CCHP, 2016).
The
hospital will need to secure RPM devices that can be handed over to the
patients. The hospital administration will also need to purchase the RPM
software, which will be installed in every physician’s computer for monitoring
their patients. Any new patient who checks in will be registered in the system
and given the RPM devices, already connected to the database. After Admission,
the patient will be taught on how to use the device by the nurse and allowed to
use it while still admitted as the nurse moves on to help other new patients.
When discharged, the patient will be instructed on how to use the device and
will be encouraged to strictly focus on their recovery. The RPM device will be
programmed to remind them when to take their medication and do other care
activities (CCHP, 2016).
References
Center for Connected Health Policy (CCHP). (2016). What is Telehealth? Available at http://www.cchpca.org/what-is-telehealth
McGonigle, D., & Mastrian, K. (2015). Nursing informatics and the foundation of knowledge (3rd ed.). Burlington, MA: Jones & Bartlett Learning.

